The Phrazer/Kitsune team, customers, partners and users are pleased to provide you with relevant and informative blog posts. Some posts are simple short text updates while others incorporate images, videos and files. Please be respectful of the bloggers, materials and goals of this offering. If you have comments and the link is disabled, please check back later.
Let’s take a look at a scenario: A provider is working in an Emergency room and is interacting with a patient through an interpreter to obtain final patient information to make a diagnosis. The provider is trying to document on the EHR while maintaining the conversation, but the computer starts lagging behind and isn’t able to access the patient’s health history. The provider has two other patients waiting to be seen and still has another 10 min of charting once the final diagnosis is made.
Sounds exhausting, right? This cycle happens multiple times over the course of a single day for a provider. It comes as no surprise that this demanding schedule is leading to burnout. The data agrees and in a recent study of U.S. physicians more than half reported experiencing at least one symptom of burnout. This is a substantial increase over previous years indicating that this kind of exhaustion among physicians and other providers is becoming a crisis.
Burnout is an experience of emotional exhaustion, depersonalization and feelings of low achievement and decreased effectiveness. Burnout has been known to be a touchy subject in the medical profession.
A high level of burnout should be considered a huge problem in the healthcare system. Stressful work conditions and exhaustion can lead to reduced empathy for patients, interpersonal relationships and patient satisfaction. It can also lead to increased medical errors, lower quality of care/patient outcomes, and more providers wanting to leave the practice. If satisfaction levels decline, the healthcare industry could see a decrease in medical school applications or students and young providers might see the stress and the toll it takes on older staff members and choose another career.
Electronic health records (EHRs) have made major impact to enhanced coordination of care and many other benefits. However, along with many of these positive improvements in technology, providers are required to learn new programs and workflows which add to the administrative burden that often is a main contributing factor in burnout. This can disrupt a provider’s daily activities and become a distraction that takes time away from face-to-face patient care.
Trying to prevent a further increase in burnout should be extremely important to the healthcare industry. By giving providers efficient tools, opportunities to decrease their stress levels, and introduce new initiatives to combat burnout healthcare organizations in turn will see increased morale which has been proven to increase the quality of patient care.
Are you burnt out? Take a look at this Mayo article to learn more: https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/burnout/art-20046642
We at GeaCom are passionate about the company’s mission: equity, efficiency, and efficacy in healthcare. We provide a truly differentiated solution that has been proven effective in the most challenging areas of care with unmatched benefits for patients, staff and system. Throughout national and international programs we have discovered that the best hardware and breakthrough methodologies are not the only factors for a successful program. Awareness of organizational change readiness, understanding the value of change and change management expertise are equally important to achieve defined goals.
Organizational Change Readiness is a complex, multi-level, multi-faceted construct that includes the entity’s commitment to change (e.g. patient equity, quality, efficiency), assignment of resources (budget, programs, etc), and is represented in culture and values. Furthermore, the urgency to change, understanding of why change is needed, ownership of change and much more are vital elements to be considered.
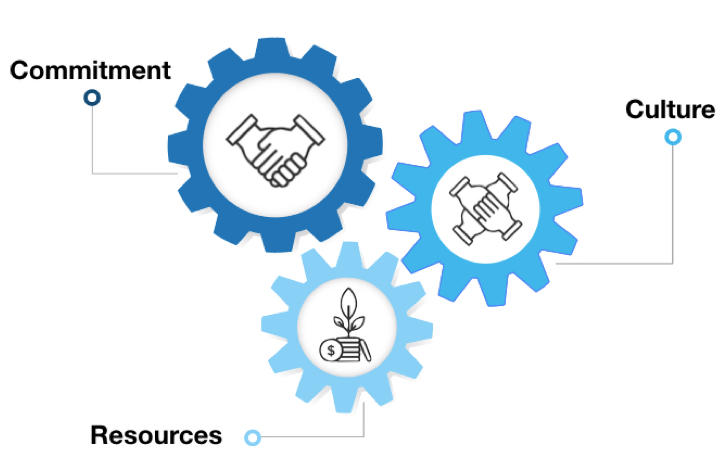 Introducing new to the world solutions and transitioning from a static method to the dynamic CITE method impacts the entire organization, its culture, processes, workflows and more. While the rewards and benefits are unprecedented we learned that to truly drive change, we need to have individuals across the organization onboard - from executives to front line staff.
Introducing new to the world solutions and transitioning from a static method to the dynamic CITE method impacts the entire organization, its culture, processes, workflows and more. While the rewards and benefits are unprecedented we learned that to truly drive change, we need to have individuals across the organization onboard - from executives to front line staff.
Establishing an understanding for the value of change and associated program requirements to realize desired benefits is vital. In the context of CITE solution this means:
- Only a fully integrated CITE program provides the breakthrough harmonization and resource 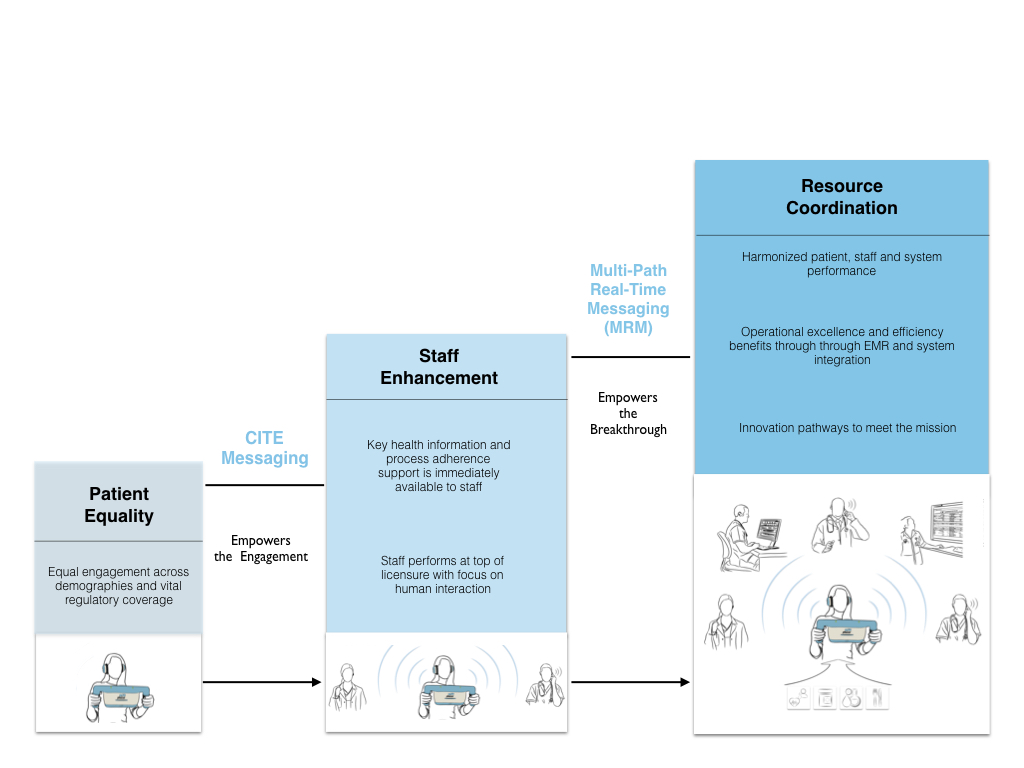 coordination benefits.
coordination benefits.
- Only a fully integrated program ensures patient equity in concert with staff top of licensure performance.
- Only a fully integrated program will pave a pathway to operational excellence, efficiency, and innovation.
- Only a fully integrated program will demonstrate the value and unfold the platforms transformation benefits.
Based on the knowledge about organizational change readiness and change management, GeaCom designs transformation programs focused on stakeholder engagement and empowerment. Champions function as internal drivers of change while endorsement and support from leadership set the framework for longterm success. Organizational goals such as the desire to establish a patient-centered model, improve efficiencies, optimize processes, accelerate innovation and establish a higher level of organizational agility are aligned with program goals. Transformative CITE solutions pave a path to modernized, equal, and effective healthcare achieved through a new level of organizational agility, adaptability and innovation.
Phrazer/Kitsune’s PEPS supports your patient-centered engagement strategy and offers a modernized and equal entertainment solution along with relevant health education and relaxation components that truly transform the patient experience.
How does it impact IT infrastructure? PEPS entertainment servers, placed inside of the internet switch, host live TV, updated media content and services that patients access without the high cost and demand of an ongoing live internet data pull for each user. The PEPS design is secure, safe, reliable, has a light network footprint and is completely configurable to each facility’s needs.
Interested in consolidating point solutions? Phrazer/Kitsune, as the only medical grade engagement solution built to FDA standards, unifies patient entertainment, nurse call system, way-finding, language services, virtual health and medical CITE engagements with strong economic benefits. The System is safe, cost-effective, fast and easier to deploy across the care continuum.
New revenue streams for your enterprise? Phrazer/Kitsune PEPS offers novel revenue avenues generated through premium entertainment and services as well as innovative sponsorship/advertisement opportunities that boost cash flows.
Phrazer/Kitsune PEPS creates a differentiated care and entertainment experiences that enhances the relationships between patients and their care communities. Furthermore, PEPS offers new efficiencies and innovation potential supporting a modern IT strategy.
The Medical CITE Journey Solution harmonizes the patient variable, ensures quality and continuity of care and  revolutionize the patient-provider interaction. The System empowers patients to take an active role in their care and author their own chart reducing charting time for staff significantly while increasing accuracy of information. Furthermore, the CITE System puts the patient back at the center, honors the individual’s preferences and values, and supports a team-based care and shared-decision making approach.
revolutionize the patient-provider interaction. The System empowers patients to take an active role in their care and author their own chart reducing charting time for staff significantly while increasing accuracy of information. Furthermore, the CITE System puts the patient back at the center, honors the individual’s preferences and values, and supports a team-based care and shared-decision making approach.
From a provider perspective, the CITE Solution reduces the burden of the EMR, support a meaningful interaction and helps resist confirmation bias. To improve the quality and avoid making decisions based on incomplete information and a variety of emotional and cognitive biases, the Systems patented Multipath Realtime Messaging (MRM) feature shares actionable, relevant information, specific to the care provider (nurse, doctor, medical assistant, etc).
CITE Solutions are easy to integrate, support providers to make better decisions with increased confidence, improve health outcomes and establish a new relationship between the patient and the provider.
 Health systems are turning towards telemedicine and virtual care platforms to improve the care process and coordinate resources more effectively. Especially smaller and rural community facilities are struggling to meet the need for specialty care.
Health systems are turning towards telemedicine and virtual care platforms to improve the care process and coordinate resources more effectively. Especially smaller and rural community facilities are struggling to meet the need for specialty care.
CITE solutions harmonize patient, staff and system performance and offer features that empower enterprises to meet their goals, for example virtual engagement capabilities for a more effective and efficient encounter.
Access to care: Access the virtual engagement features quickly and easily without interrupting the care process. Consult with any specialist including infectious disease experts, mental health providers, social workers and more. Relevant, actionable information about the patient gathered through CITE engagements are available to the specialist for a more meaningful interaction.
Improve patient flow and experience: Utilize the System’s virtual engagement capabilities to improve patient flow, access to care and experience while reducing waiting times for patients significantly. For example: inside a care facility, the discharge or admission of the patient can be supported virtually via staff on site or remotely. The provider can be in the same facility, in a different facility within the region, at home, or in a different province and easily connect with the patient via Phrazer/Kitsune using a computer or other electronic device. This opens up new opportunities for providers to engage beyond their office hours, to utilize specialists more effectively and improve outcomes. Outside of care facilities, Phrazer/Kitsune as a journey solution supports chronic patients in their homes with synchronous and asynchronous engagements and staff is able to monitor patients’ progress eliminating the need for office visits.
Lower the cost of care: Managing resources and patient flow more effectively offers financial benefits to the health system. Reduce the cost of care with improved throughput, reduction of LoS, increased compliance with the care plan, and consolidation of costly point solutions. Explore novel reimbursements for virtual engagements and ensure patient and staff safety by utilizing the world’s only medical grade engagement solution, Phrazer/Kitsune, and breakthrough CITE Methodologies.
The importance of mental health is expanding at a rapid rate as we further understand how both mental and physical health are important in creating healthy populations. It has been mentioned in our previous blog posts that putting effort towards preventative care (Screening and Brief Interventions) can lead to drastic health improvements and major cost avoidance down the road for patients.
Check out the past SBIRT Post: A few reasons why you should perform SBIRT activities
Here, we are going to focus on screening for depression and dive into when screening should start, how we can focus on younger populations and how often screening should take place.
When should we start screening for depression?
Looking at information available through numerous studies we need to start earlier than we previously thought (i.e. adolescents) to catch illnesses before they manifest into much larger, complex issues.
Teenage depression is a serious mental illness that affects millions of teenagers in the United States each year while only a small portion of affected teens ever get professional help. The STAR*D (Sequenced Treatment Alternatives to Relieve Depression) study found that nearly 40 percent of youth had their first depressive episode before the age of 18. (1)
How do we start screening adolescents?
There is a screener available for younger patients (12-17 years of age) called the PHQ-9 Modified for Adolescents or the PHQ-A. This screening tool can be used in healthcare, schools or other appropriate settings these serious topics can be approached.
It’s important to keep in mind that depression in adolescents can reveal itself in very different ways compared to older individuals. The following symptoms of depression are more common in teenagers than in their adult counterparts.
- Irritable or angry mood - Irritability, rather than sadness, is often the predominant mood in depressed teens. A depressed teenager may be grumpy, hostile, easily frustrated or prone to angry outbursts.
- Unexplained aches and pains - Depressed teens frequently complain about physical ailments such as headaches or stomach aches. If a thorough physical exam does not reveal a medical cause, these aches and pains may indicate depression.
- Extreme sensitivity to criticism - Depressed teens are plagued by feelings of worthlessness, making them extremely vulnerable to criticism, rejection and failure. This is a particular problem for “overachievers.”
- Withdrawing from some people, but not all - While adults tend to isolate themselves when depressed, teenagers usually keep up at least some friendships. However, teens with depression may socialize less than before, pull away from their parents, or start hanging out with a different crowd.
How often should we screen?
At a minimum, patients of all ages should be screened on an annual basis. Results should be documented in the EHR and tracked for changes each time a new screening is performed. We realize this may not be a reality for all patients and practices, but screening early and often has proven to promote safer, healthier populations and reduce future costs.
When it comes to billing for mental health we have found that CPT 96127 can be used “when medically necessary” up to 4 units per visit. Reimbursement levels can vary (~$4-25) so we recommend working with your billing team to understand the intricacies of the billing process and potential impact to your practice.
In conclusion
Screen early and screen often; early action by the care network can have lasting benefit for young individuals. As children develop, depression can evolve and present itself in ways that are different from adults and it’s the job of the care network to identify any issues and support the well-being of the individual.
1. American College of Preventive Medicine (2009, October 6). Primary Care Urged to Have Systems in Place for Screening and Treating Depression. ScienceDaily
 As reimbursement models and care delivery shift towards patient centered and value based journey solutions, health systems are challenged with the operationalization. While conventional methods reached the ceiling and only provide limited results in one category, CITE solutions, as the world’s only medical grade engagement system, enable enterprises to:
As reimbursement models and care delivery shift towards patient centered and value based journey solutions, health systems are challenged with the operationalization. While conventional methods reached the ceiling and only provide limited results in one category, CITE solutions, as the world’s only medical grade engagement system, enable enterprises to:
- Engage all patients equally and meet civil right requirements
- Encourage top of licensure performance and reduce charting time
- Empower system innovation, efficiency and revenue pathways
As the only holistic engagement solution, Phrazer/Kitsune harmonizes patient, staff and system performance. CITE systems offer personalized engagements for your patient population with continuity and quality across demographies. The patented MRM feature supports a care dialogue between patients and staff with actionable information and procedural guidance resulting in effective coordination of resources. Departments and the entire organization are empowered to innovate at no additional cost, boost current and future initiatives and establish a new level of patient experience, health outcomes, staff performance and system operation. A truly transformative solution for patient equity, efficiency, and efficacy.
Let’s start with one fact.
For every dollar spent on screening for substance use and providing early intervention approximately $4 can be saved in healthcare costs. (1)
Quick Recap on what SBIRT is:
Screening, Brief Intervention and Referral to Treatment (SBIRT) is an evidence-based approach to identifying patients who use alcohol and other drugs at risky levels, and in turn reduces and prevents related health consequences, disease, accidents and injuries.
SBIRT is unique in that it screens for all types of substance use, not just dependencies. Each part of the SBIRT process provides information and assistance tailored to the patient’s needs.
The primary goal of SBIRT is not to identify alcohol or other drug dependent individuals, but rather, it is intended to meet the public health goal of reducing the harms and societal costs associated with risky use.
Why isn’t everyone doing it?
Well the simple answer is, multiple reasons. Time constraints and cost are two prominent factors that are always present when trying to incorporate additional activities into the care process.
In a typical family practice, providers usually have between 10-15 minutes with a patient. This isn’t anything new. Healthcare professionals already know it’s incredibly challenging to give the patient the time they need to address the initial reason for the visit, much less anything that may come up while the patient has the provider’s attention (insert patient statement “oh and I have this thing on my back, could you look at it?”). How can you expect to do more without increasing the time per patient?
When considering cost, every health organization is on a budget so optimizing every dollar to provide the maximum benefit is critical. You’re already working on a budget, and giving a dollar to a new activity can often mean taking a dollar away from some other part of care. Again, this isn’t new, but it is the harsh reality of operating a health system. So, how do you accomplish more with the same or even less budget?
A Solution to Starting SBIRT Activities
Many health organizations are looking to technology that can automate the information gathering process and provide a summary to staff for quick review. Typically they are looking for a technology that has low overhead, requiring no additional outside resources, and can be set up quickly in existing workflows to start engaging patients.
Setting Phrazer up for a patient engagement takes ~30 seconds and can be completed by an intake staff member (or the patient in some workflows). Then simply allow the patient to begin screening activities in the waitroom or wherever the patient will have wait time to complete.
With the CITE Engagements on Phrazer, patients don’t need to be able to read or write to complete and Phrazer can screen in any patient language (English, Spanish, Somali, Hmong, American Sign Language or any other language, you name it).
Phrazer actually educates the patient how to use as they start their interactions. The patient simply follows the onscreen provider and interacts with the touchscreen to enter their answers.
The patient follows a branching system to reduce survey fatigue so the patient is only asked questions that are relevant to them based on previous answers. (For example if they don’t drink alcohol, they only perform the AUDIT-C and don’t move on to complete the full AUDIT)
It is key to point out is that the patient is doing all the screening on their own without training on the device and requires no additional staff time. Outside of basic setup in some workflows you are able to completely gather this valuable information with minimal employee expenditure.
Patients typically take from 5-15 minutes to complete and when a patient is done, Phrazer generates a patient summary (See Below for example), including scores for each screener, based on the patient answers for staff to utilize during the care process.
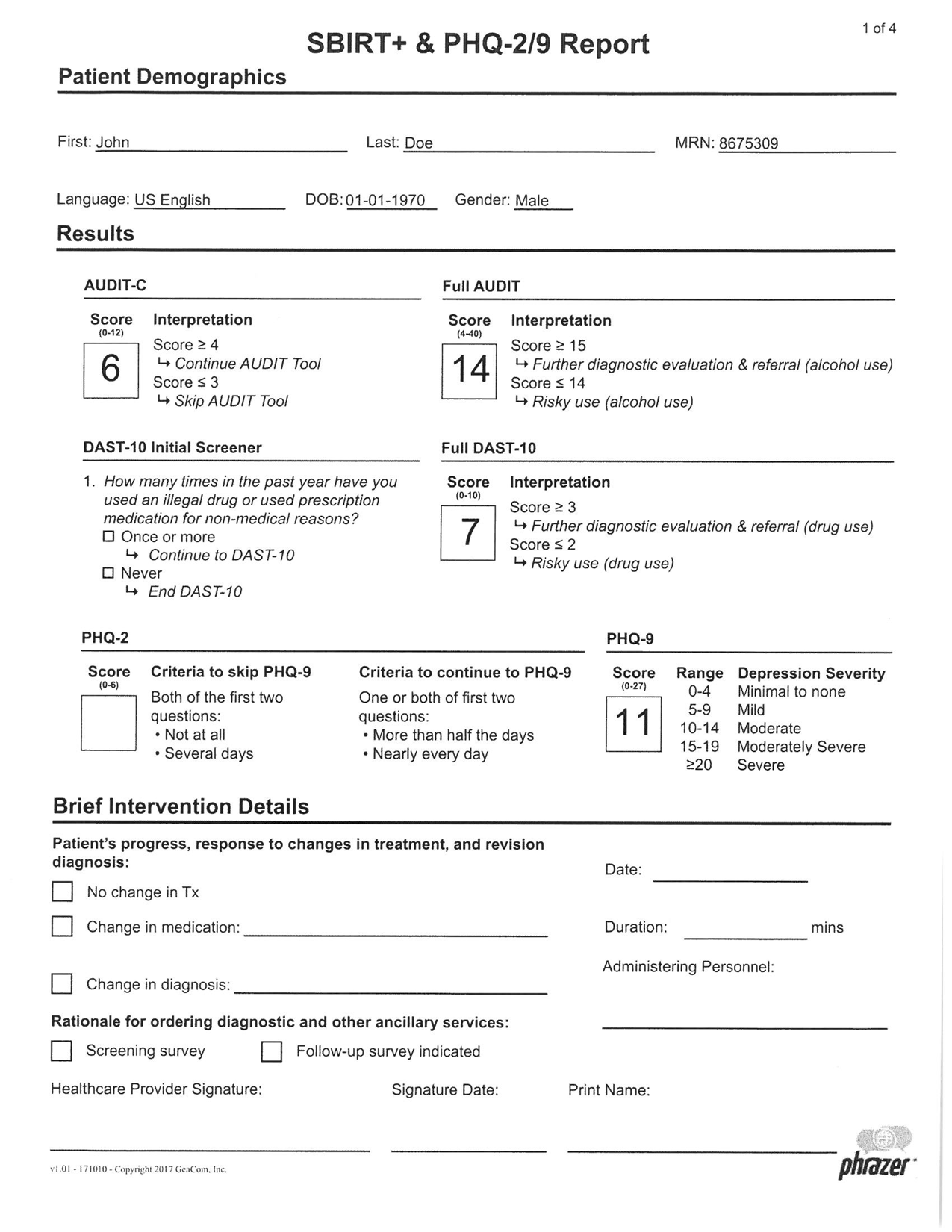

These printouts travel with the patient, via the electronic record or paper copies, and providers can review before walking into the room with the patient. The goal is to give relevant information to the provider to identify and have meaningful conversations with at risk patients without becoming a time burden on staff. With technology, this goal is realistic with solutions that fit into the existing workflow without disruption.
Once care is provided to the patient and the provider signs off on the care provided, the records along with recommended billing codes travel to the billing team for reimbursement. Reimbursement is pushed using the patient’s health insurance (private insurance, medicare, medicaid) and in the following days, reimbursement is sent to your facility.
Through the use of technology you can reduce the cost and time burden of implementing new or upgrading existing SBIRT activities.
Let’s recap a few reasons why you should be providing SBIRT services:
1. It’s proven that preventative care including SBIRT activities reduces the overall cost of healthcare
2. You will be providing more holistic care to your patients based on additional screening information meaning a safer, healthier population
3. Insurance typically covers the cost of care and increasing your billable dollars can assist with your bottom line
If you’re curious to learn more about how existing health systems have adopted a technology approach to operationalize new processes, let us know, we would be happy to share more about our experience. Email info.sbirt@geacom.net
For more information on how to implement SBIRT in primary care, check out this NCBI study: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5809898/
(1) Fleming, M. F., Mundt, M. P., French, M. T., Manwell, L. B., Stauffacher, E. A., & Barry, K. L. (2000). Benefit-cost analysis of brief physician advice with problem drinkers in primary care settings. Medical Care, 38(1), 7–18.
